55 yrs old Male with sob since 20 days
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case i have seen:
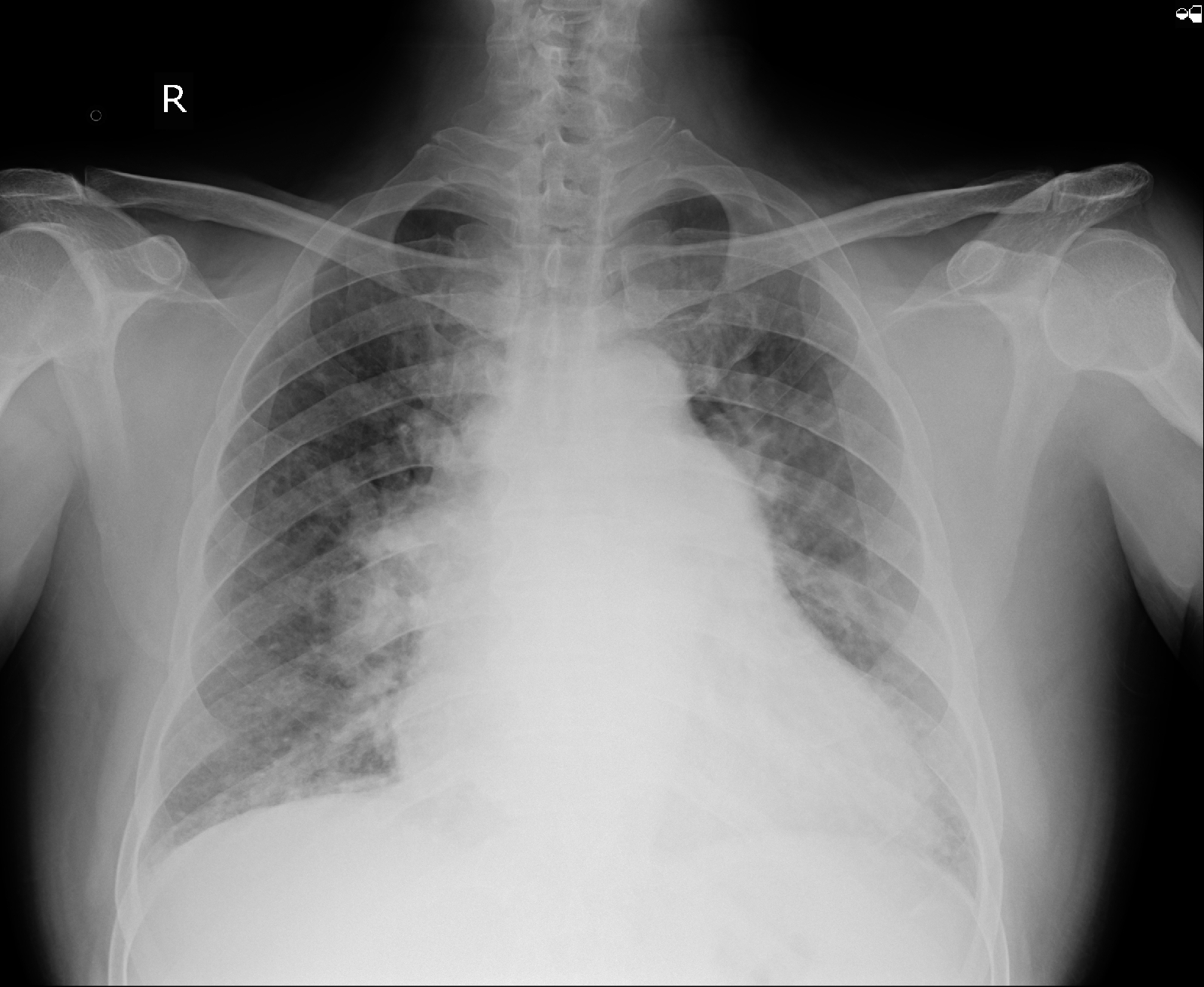
55 year old male patient,farmer by occupation came with c/o sob (grade2 to grade 3) according to NYHA classification since 20 days
C/o cough since 20 days
C/o pedal edema since 20 days
C/o fever since 7 days
Patient was apparently asymptomatic 3 yrs ago(in 2017) then he developed Sob which exaggerated on working and walking for long distance in the fields and cough ,which is progressive in nature, associated with sputum(yellowish in color) non foul smelling and not associated with blood. He went to a cardiologist where he is diagnosed with hypertension and got treated accordingly and he was recovered after taking medications.
20 days back he came to OPD with c/o SOB (grade 2 to grade 3) according to NYHA associated with giddiness and orthopnoea ,not associated with palpitations or heaviness in chest and PND .
C/o cough since 20 days gradual in onset ,progressive in nature ,associated with sputum (yellowish in colour ) ,non foul smelling ,small consistency not associated with blood
C/o pedal edema since 20 days (pitting type ),gradually progressive up to knee.
H/o fever (gradual in onset ,progressive in nature )present through out the day associated with chills and rigors and subsided on taking medications .
H/o varicosities on the Medial aspect of Rt.leg and thigh associated with edema progressive to generalised ,not associated with pain and itching.
K/c/o HTN (on regular medications since 3 years )
K/c/o alcoholic and smoker since 30 years (90 to 100 ml per day and smokes 3 packs of beedies per day )
No h/0 CAD ,asthma,tuberculosis , epilepsy ,thyroid or any surgeries
GENERAL EXAMINATION:
O/E Pt is c/c/c moderately nourished and well built well oriented to time person place.
Vitals
BP : 120/80 mmhg
RR:20 cpm
PR: 72bpm
Temp: 98.6 F
Cvs:s1,s2heard ,jvp normal, jvp raised prominent on sitting and sleeping position.
RS:Decreased breath sounds on right and left infrascapular.
CNS: NAD
P/A : soft ,non tender ,bowel sounds present .
Referred to surgery:
On local examination :
Blackish discoloration around Rt ankle joint.
No ulcers seen.
Both limbs are symmetrical in size.
B/l sensory and motor system normal
No limb deformity
Trendenberg test 1 and 2 are positive
Diagnosis:Rt lower limb varicosities involving GSV Teritory without complications.
Advice:
1) Grade -3 stockings
INVESTIGATIONS:
Hemogram:
HB-16.5gm/dl
TC-8,200cells/cumm
PCV-51.3 vol%
MCV-80.6 fl
PC-1.60 lakh/cu.mm
Troponin-I = Negative
T3 - 0.70 ng/ml
T4 - 10.00 micro g/dl
TSH - 2.55 micro lu/ml
ECG:
Diagnosis :
HFpEF with EF -58% Rt.Heart failure secondary to COPD with severe PAH -type 2 with AKI
Treatment:
Day1
1) Inj.lasix 80mg IV/stat
Inj . Lasix 40 mg IV/TID
2)Head end elevation.propped up position.
3)Syrup.Ascoril 10ml/TIB
4)Tab.Amlong 5mg/PO/OD@8am
5) Nab with Asthalin 8th hourly
Mucomist 12th hourly
6)Strict I/O Charting hourly
7)Bp/PR/Temp hourly
8)Fluid Restriction less than 1.5 lit/day
9)Salt Restriction less than 2g/day
10)oxygenation if required
11)wt monitoring daily
DAY2,3,4,5
1) Inj.lasix 40 mg/IV/BD
2) Syrup.Ascoril 10ml/PO/BD
3) Nab With Asthalin 6th hourly and budecord 12th hourly
4)Tab.Amlong 5mg/PO/OD@8am
5)Strict I/O Charting hourly
6)Bp/PR/Temp hourly
7)Fluid Restriction less than 1.5 lit/day
8)Salt Restriction less than 2g/day
9)Daily at.monitoring
10)Grade -3 stocking.















Comments
Post a Comment